Day 1 :
Keynote Forum
Lee Hyer
Georgia Neurosurgical Institute, USA
Keynote: New model: Holistic assessment and treatment of older adults
Time : 09:00-09:35

Biography:
Abstract:
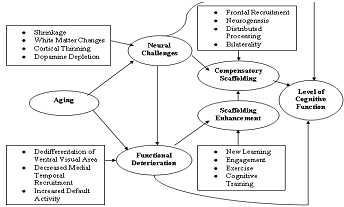
Neural Enrichment & Neural Depletion

Keynote Forum
Angela Kydd
Edinburgh Napier University, UK
Keynote: Prescribing for the oldest old
Time : 09:35-10:10

Biography:
Abstract:
Keynote Forum
Stephen Jacobs
University of Auckland, New Zealand
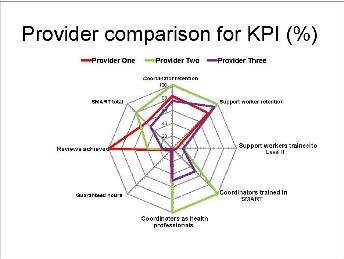
Keynote: A systematic method for improving service quality in home support services for older people
Time : 10:10-10:45

Biography:
Abstract:
- Jacobs SP, Rouse P, Parsons M (2014) Leading change within health services: The theory behind a systematic process for leading the implementation of new services within a network structure. Leadership in Health Services 27,2:72-86
- Senior HE, Parsons M. Kerse N, Chen M, Jacobs S, Vanderhoorn, S, Anderson C. (2014) Promoting independence in frail older people: a randomised controlled trial of a restorative care service in New Zealand. Age & Ageing 43: 418–424
- Parsons, M, Anderson C, Senior H, Chen X, Kerse N, Jorgensen D, Brown p, Jacobs S, Vanderhoorn S, Kilpatrick J. (2005) ASPIRE - Assessment of Services Promoting Independence and Recovery in Elders. Auckland: The University of Auckland.
- Sajtos, L., Rouse, P., Harrison, J., & Parsons, M. (2014). Case-mix system as a boundary object: the case of home care services. Australasian Marketing Journal (AMJ), 22 (3), 189-196.
- Breitenstein, S.M., Gross, D., Garvey, C.A., Hill, C., Fogg, L. and Resnick, B. (2010) Implementation fidelity in community-based interventions, Research in Nursing and Health, 33, 164-173.

- Elderly Care | Gerontological Nursing | Geriatric Medicine | Geriatric Case Studies | Geriatric Dementia | Geriatric Mental Health | Geriatrics Palliative Care
Location: Balvenie Glenmorangie

Chair
Lee Hyer
Georgia Neurosurgical Institute | USA

Co-Chair
Stephen Jacobs
University of Auckland | New Zealand
Session Introduction
Vigdis Abrahamsen Grøndahl
Østfold University College, Norway
Title: Health care quality from the persons with dementia’s perspective: Development and testing of a questionnaire
Time : 11:10-12:50

Biography:
Abstract:
- Drageset J, Kirkevold M. Espehaug B. (2011). Loneliness and social support among nursing home residents without cognitive impairment: A questionnaire survey. Int J Nurs Stud, 48:611–619.
- Helgesen AK (2013). Patient participation in everyday life in special care units for persons with dementia. Faculty of Social and Life Sciences, Karlstad University Studies. (Doctoral dissertation).
- Larsson G, Wilde-Larsson B. (2001). Quality of care and service as perceived by adults with developmental disabilities, their parents and primary caregivers. Mental Retardation 39:249-258.
- Perales J, Cosco TD, Stephan BC, Haro JM, Brayne C. (2013) Health-related quality-of-life instruments for Alzheimer's disease and mixed dementia. International Psychogeriatrics, 25:691-706.
- van Baalen A, Vingerhoets Ad JJM, Sixma HJ & de Lange J (2011). How to evaluate quality of care from the perspective of people with dementia: an overview of the literature. Dementia, 10:112–37.
Ann Karin Helgesen
Østfold University College, Norway
Title: Health care quality from the persons with dementia’s perspective: Development and testing of a questionnaire
Time : 11:10-12:50

Biography:
Abstract:
- Drageset J, Kirkevold M. Espehaug B. (2011). Loneliness and social support among nursing home residents without cognitive impairment: A questionnaire survey. Int J Nurs Stud, 48:611–619.
- Helgesen AK (2013). Patient participation in everyday life in special care units for persons with dementia. Faculty of Social and Life Sciences, Karlstad University Studies. (Doctoral dissertation).
- Larsson G, Wilde-Larsson B. (2001). Quality of care and service as perceived by adults with developmental disabilities, their parents and primary caregivers. Mental Retardation 39:249-258.
- Perales J, Cosco TD, Stephan BC, Haro JM, Brayne C. (2013) Health-related quality-of-life instruments for Alzheimer's disease and mixed dementia. International Psychogeriatrics, 25:691-706.
- van Baalen A, Vingerhoets Ad JJM, Sixma HJ & de Lange J (2011). How to evaluate quality of care from the perspective of people with dementia: an overview of the literature. Dementia, 10:112–37.
- Wilde Larsson, B. and Larsson, G. (2002), “Development of a short form of the Quality from the patient’s perspective (QPP) questionnaire”, Journal of Clinical Nursing, Vol. 11 No. 5, pp. 681-687.
Liv Berit Fagerli
Østfold University College, Norway
Title: The impact of person-centered care on older people’s perceptions of care quality in nursing homes: An intervention study
Time : 11:10-12:50

Biography:
Abstract:
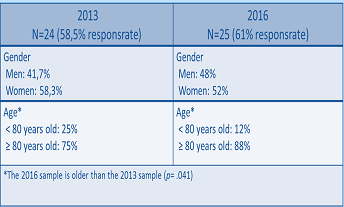
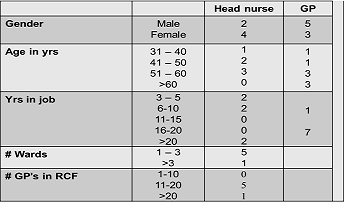
Sample characteristics
- Askari M, Wierenga PC, Eslami S, Medlock S, Rooij SE, Abu-Hanna A (2011) “Assessing quality of care of elderly patients using the ACOVE quality indicator set: a systematic review”, PLoS ONE, Vol. 6 No. 12, e28631.
- Backhaus R, Verbeek H, van Rossum E, Capezuti E, Hamers JPH (2014) “Nurse staffing impact on quality of care in nursing homes: a systematic review of longitudinal studies”, Journal of the American Medical Directors Association, Vol. 15 No. 6, pp. 383-93.
- Grøndahl VA, Fagerli LB Nursing home care quality: a cluster analysis. International Journal of Health Care Quality Assurance. (in press)
- Hasson H, Arnetz JE (2010) “A comparative study of nursing staff, care recipients’ and their relatives’ perceptions of quality of older people care”, International Journal of Older People Nursing, Vol. 5 No. 1, pp. 5-15.
- Hughes K, Moore S (2012) “Quality of life versus quality of care: elderly people and their experience of care in South Australian residential facilities”, Practice: Social Work in Action, Vol. 24 No. 5, pp. 275-285.

Eli-Anne Skaug
Østfold University College, Norway
Title: Male residents’ experiences of an activity program for men only in a nursing home
Time : 11:10-12:50

Biography:
Abstract:
- Bradshaw SA, Playford ED, Riazi A (2012) Living well in care homes: a systematic review of qualitative studies. Age and Ageing, 41(4), 429-440.
- den Ouden M, Bleijlevens M, Meijers JM, Zwakhalen SM, BraunSM, Tan FE, Hamers JP (2015). Daily (In) Activities of nursing home residents in their wards: an observation study. Journal of the American Medical Directors Association, 16(11), 963-968.
- Helgesen AK (2013). Patient participation in everyday life in special care units for persons with dementia. Faculty of Social and Life Sciences, Karlstad University Studies. (Doctoral dissertation).
- Helgesen AK, Skaug EA, Abrahamsen Grøndahl V (2016) Changing Men’s Everyday Lives in Nursing Homes: A Grounded Theory Study. The International Journal of Person Centered Medicine 2016 Vol 6 Issue 3 pp 185-190.
- Moss, SZ, Moss MS (2007). Being a man in long term care. Journal of Aging Studies, 21(1), 43-54.
Ann Karin Helgesen
Østfold University College, Norway
Title: User participation in everyday decision-making in special care units for persons with dementia
Time : 11:10-12:50

Biography:
Abstract:
- Boer M, Hertogh C, Droes RM, Riphagen I, Jonker C, Eefsting J (2007) Suffering from dementia – the patient’s perspective: a review of the literature. International Psychogeriatrics 19, 1021–1039.
- Cahill J (1998) Patient participation – a review of the literature. Journal of Clinical Nursing 7, 119–128.
- Helgesen AK (2013) Patient participation in everyday life in special care units for persons with dementia. Faculty of Social and Life Sciences, Karlstad University Studies. (Doctoral dissertation).
- Menne HL, Whitlatch CJ (2007) Decision-making involvement of individuals with dementia. The Gerontologist 47, 810–819.
- Wilkinson H (2001) Empowerment and decision-making for people with dementia: the use of legal interventions in Scotland. Ageing & Mental Health, 5, 322–328.
Vigdis Abrahamsen Grøndahl
Østfold University College, Norway
Title: Older people’s involvement in activities related to meals in nursing homes
Time : 11:10-12:50

Biography:
Abstract:
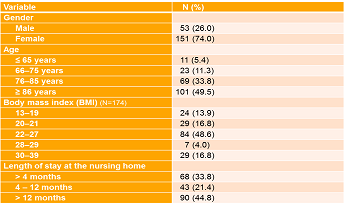
Table 1a. Characteristics of the residents (N=204)
Recent Publications:
- Beattie E, O’Reilly M, Strange E, Franklin S, Isenring E (2014) How much do residential aged care staff members know about the nutritional needs residents? International Journal of Older People Nursing 9, 54-64.
- Carrier N, West GE, Ouellet D (2009) Dining experience, food services and staffing are associated with quality of life in elderly nursing home residents. The Journal of Nutrition, Health & Aging 13, 565-570.
- Divert C, Laghmaoui R, Crema C, Issanchou S, Van Wymelbeke V, Sulmont-Rossé C (2015) Improving meal context in nursing homes. Impact of four strategies on food intake and meal pleasure. Appetite 84,139-147.
- Grøndahl VA, Aagaard H (2016) Older people’s involvement in activities related to meals in nursing homes. International Journal of Older People Nursing 11, 204-213.
- McCormack B, Dewing J, McCance T (2011) Developing person-centred care: Addressing contextual challenges through practice development. Online Journal of Issues in Nursing 16(2).
Bart Van Rompaey
University of Antwerp, Belgium
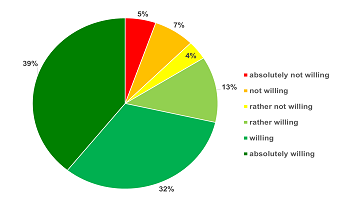
Title: Transmural cooperation between general practioners and nursing staff in residential care facilities
Time : 12:50-13:15

Biography:
Abstract:
- Vanwesemael T, Van Rompaey B, Petrovic M, Boussery K, Dilles T. SelfMED: Self-Administration of Medication in hospital. A prevalence study in Flanders, Belgium, Journal of Advanced Nursing, (2016), 72,58-9
- Bogaerts A, De Baetselier E, Ameye L, Dilles T, Van Rompaey B, Devlieger R, Postpartum weight trajectories in overweight and lean women, Midwifery,2016, 1-19
- Mestdagh E, Van Rompaey B, Beeckman K, Bogaerts A, Timmermans O, A concept analysis of proactive behaviour in midwifery, J Adv Nur-2016, 72(6), 1236-1250
- Van Bogaert P, Peremans L, Diltour N, Van heusden D, Dilles T, Van Rompaey B, Sullivan Havens D, Staff nurses' perceptions and experiences about structural empowerment: a qualitative phenomenological study PLoS ONE,2016, 11 (4)
- Van Rompaey B, Van Hoof, A; Van Bogaert P; Timmerman, O; Dilles T, The patients' perception of a delirium: a qualitative research in a Belgian intensive care unit, Intensive Crit Care Nurs, 2016 Feb;32:66-74

Libba Reed McMillan
Auburn University, USA
Title: Integration of end of life care of military members and veterans into a baccalaureate nursing concepts course
Time : 14:00-14:25

Biography:
Abstract:
- Boss, P. (1999). Ambiguous loss--Learning to live with unresolved grief. Harvard University Press, Cambridge, MA.
- Breen, L. (2012). The effect of caring on post-bereavement outcome: research gaps and practice priorities. Progress in palliative care, 20(1), 27-30.
- Burke, L., Clark, K., Ali, K., Gibson, B., Smigelsky, A. & Neimeyer, R. (2015). Risk factors for anticipatory grief in family members of terminally ill Veterans receiving palliative care services. Journal of social work in end-of-life and palliative care. 11:244-266.
- Grassman, D. “Wounded warriors: Their last Battle”, Home healthcare Nurse. 25 (5): 299-304, May 2007
- Hynes, C. & Thomas, M. (2016). What does the literature say about the needs of veterans in the areas of Health? Nurse Education Today, 47, 81-88.
Tinne Dilles
University of Antwerp, Belgium
Title: Self-administration of medication in hospital: A mixed-method study on the perspectives of patients and health care providers
Time : 14:25-14:50

Biography:
Abstract:
- Vanwesemael, T., Van Rompaey, B., Petrovic, M., Boussery, K., & Dilles, T. (2017). SelfMED: Self-Administration of Medication in Hospital: A Prevalence Study in Flanders, Belgium. J Nurs Scholarsh. 2017 May;49(3):277-285.
- Willemse E., Anthierens S., Farfan-Portet MI., Schmitz O., Macq J., Bastiaens H., Dilles T., Remmen R. (2016) Do informal caregivers for elderly in the community use support measures? A qualitative study in five European countries. BMC Health Serv Res. 2016 Jul 16;16:270.
- Paque K, Goossens K, Elseviers M, Van Bogaert P, Dilles T. (2016) Autonomy and social functioning of recently admitted nursing home residents. Aging Ment Health. 2016 May 13:1-7.
- Dilles T, Van Rompaey B, Van Bogaert P, Elseviers MM. (2015) Resident and nurse reports of potential adverse drug reactions. Eur J Clin Pharmacol. 2015 Jun;71(6):741-9
- Van Bogaert P, Tolson D, Eerlingen R, Carvers D, Wouters K, Paque K, Timmermans O, Dilles T, Engelborghs S. (2016) J Psychiatr Ment Health Nurs. 2016 Nov;23(9-10):568-575.

Chanel Burke
University of Technology Sydney, Australia
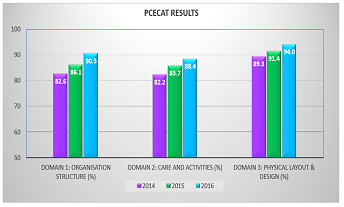
Title: Improving quality of life for people with dementia: The Person-Centred Environment and Care Assessment Tool
Time : 14:50-15:15

Biography:
Abstract:
- Edvardsson et al. (2008). Person-centred care of people with severe Alzheimer’s disease: current status and ways forward. Lancet Neurology, 7(4), 362-367.
- Commonwealth Department of Health and Family Services (1998). Standards and Guidelines for Residential Aged Care Services Manual. Commonwealth Department of Health and Family Services, Aged and Community Care Division, Canberra.
- Kitwood T. (1997) Dementia Reconsidered: The person comes first. Open University Press, Buckingham.
- Burke C, Stein-Parbury J, Luscombe G, Chenoweth L. (2016) Development and Testing of the Person- Centre Environment and Care Assessment Tool (PCECAT). Clinical Gerontologist Vol 39, ISS. 4.

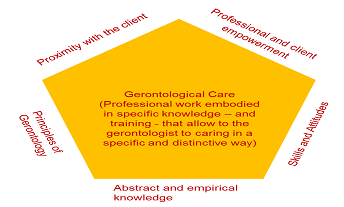
Fernando Pereira
Institute Polytechnic of Braganca, Portugal
Title: Gerontologist skills and client satisfaction in long-term residential care for older persons
Time : 15:15-15:40

Biography:
Abstract:
- Falcão, A., Pereira, F., Pimentel, H., Teixeira, C., & Rodrigues, V. (2016). The academic background of gerontologists and client satisfaction in long-term residential care for older persons. Educational Gerontology, 1–11.
- Caria, Telmo H., & Pereira, Fernando (2016). Social work like as a bureaucratic professional labour: An empirical analysis in non-profit organizations in Northern Portugal. European Journal of Social Work, 19(1), 120-139.
- Fernando Pereira e Telmo Caria (2014). “Travail professionnel des gérontologues: une approche méthodologique”. Revista Le Sociographe. Champ Social Éditions. pp 306-330.
- Fernando Pereira (Coordinator) (2017) "Theory and Practice of Gerontology: A Guide for Caregivers of Elderly". Second Edition. Ed. Psicosoma, Viseu.
- Fernando Pereira and Celeste Antão (2013) "Concept of Gerontological Care Professionals Provided by gerontologists". International Journal of Development and Educational Psycology INFAD Journal of Psychology. Year XXV, No. 2-2013. p. 51-58.

Yannic van Gils
University of Antwerp, Belgium
Title: Drinking motives of community dwelling older adults and its associated factors
Time : 15:40-16:05

Biography:
Abstract:
- Cooper ML, Russell M, Skinner JB, Windle M (1992) Development and validation of a Three-Dimensional Measure of Drinking Motives Psychological Assessment 4:123-132
- Gilson KM, Bryant C, Bei B, Komiti A, Jackson H, Judd F (2013) Validation of the Drinking Motives Questionnaire (DMQ) in older adults Addict Behav 38:2196-2202 doi:10.1016/j.addbeh.2013.01.
- Hoeck S, Van Hal G (2013) Unhealthy drinking in the Belgian elderly population: prevalence and associated characteristics European Journal of Public Health 23:1069-1075 doi:10.1093/eurpub/cks152.
- Immonen S, Valvanne J, Pitkala KH (2011) Older adults' own reasoning for their alcohol consumption International journal of geriatric psychiatry 26:1169-1176 doi:10.1002/gps.2657
- Rehm J., Gmel G., Gmel G., Hasan O., Imtiaz S., Popova S., Probst C., Roerecke M., Room R., Samokhvavlov A., Shield K & Shuper P. (2017) The relationship between different dimensions of use and the burden of disease – an update. Addiction. 1:1-34
Alba Malara
National Association of Third Age Residences (ANASTE), Italy
Title: Profiles of ICF disability in Alzheimer and vascular dementia
Time : 16:25-16:50

Biography:
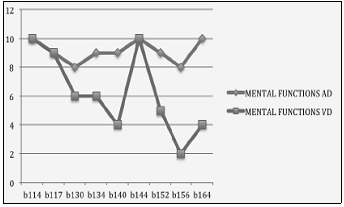
Abstract:
- World Health Organization.: International Classification of Functioning, Disability and Health : ICF. Geneva, World Health Organization; 2001.
- Ustun B: The international classification of functioning, disa- bility and health-a common framework for describing health states. 2002. http:// whqlibdoc.who.int/publications/2002/9241545518_Chap7.3.pdf.
- Mueller M, Lohmann S, Strobl R, Boldt C, Grill E. Patients’ functioning as predictor of nursing workload in acute hospital units providing rehabilitation care: a multi-centre cohort study. BMC Health Services Research 2010; 10:295- 307
- Okochi J, Utsunomiya S, Takahashi T. Health measurement using the ICF: Test-retest reliability study of ICF codes and qualifiers in geriatric care. Health and Quality of Life Outcomes 2005; 3:46-59
- Mueller M, Boldt C, Grill E, Strobl R, Stucki G: Identification of ICF categories relevant for nursing in the situation of acute and early post- acute rehabilitation. BMC Nurs 2008; 7:3.

Lisa PL Low
Caritas Institute of Higher Education, Hong Kong
Title: Opting out of own homes for residential care homes: Decision-making experiences of family members of older adults with moderate dementia
Time : 16:50-17:15

Biography:
Lisa PL Low works as an Associate Professor. Her research interests are gerontology and long-term care, with emphasis on the organization of gerontological care and practices, discharge planning for older patients and family members. Her Ph.D. thesis adopts a constructivist grounded theory approach to explore decisionmaking in residential care homes from the perspectives of older residents, family members and care providers. This work has now been extended to explore family decision-making of older people with mild-moderate dementia and for clients with intellectual disability using predominately qualitative research approaches. As part of her post-doctoral development her intentions are to continue to develop qualitative research approaches and methodologies in her academic and research career.
Abstract:
- Low LPL, Lam LW, Fan KP (2017) Decision-making experiences of family members of older adults with moderate dementia towards community and residential care home services: A grounded theory study protocol. BMC Geriatrics (accepted).
- Low LPL, Fan KP (2016) Sampling issues using the grounded theory methodology: Applicability to family caregiving research of clients with dementia and intellectual disability. 15th Qualitative Methods Conference 3-5 May: 24.
- Low LPL, Fan KP (2015) Contested provocation: Reflected experiences of the lives of family caregivers before the admission of older residents with dementia. 22nd Annual Congress of Hong Kong Association of Gerontology 21 Nov: 43.
- Low LPL, Lam LW (2013) Decision-making role, potential and challenges faced by family members when making decisions for residential care home residents with mild to moderate dementia. 16th Asia Pacific Regional Conference of Alzheimer’s Disease International 11-13 Dec: 24.
Beyhan Cengiz Ozyurt
Ege University, Turkey
Title: Assessment of risk of falls in the elderly and associated factors with falls
Time : 17:15-17:25

Biography:
Abstract:
- Deandrea S, Lucenteforte E, Bravi F, et all (2010) Risk Factors for Falls in Community-dwelling Older People: "A Systematic Review and Meta-analysis, Epidemiology 21(5):658-668
- Laurence Z. Rubenstein (2006) Falls in older people: epidemiology, risk factors and strategies for prevention, Age and Ageing; 35-S2
- Moylan KC, Binder EF,Falls in Older Adults: Risk Assessment, Management and Prevention (2007) The American Journal of Medicine 120(6):493.e1–493.e6
- Chang T, Morton S, Rubenstein L, (2004) Interventions for the prevention of falls in older adults: systematic review and meta-analysis of randomised clinical trials BMJ (328):1-7
- Lord, SR Sherrington C, Menz HB (2007), Falls in older people: risk factors and strategies for prevention, Cambridge University Press

Guillaume Souesme
Francois Rabelais University, France
Title: What is an autonomy supportive environment in geriatric care services for healthcare professionals?
Time : 17:25-17:35

Biography:
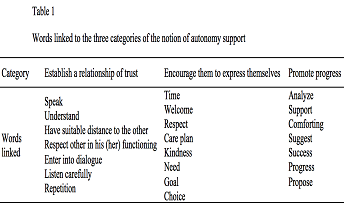
Abstract:
- Deci EL, & Ryan RM (1985) Intrinsic motivation and self-determination on human behavior. New-York: Plenum Press.
- Patton MQ (2002) Qualitative research and evaluation methods. Thousand Oaks, CA: Sage Publications Inc.
- Reeve J (1998) Autonomy support as an interpersonal motivating style. Is it teachable? Contemporary Educational Psychology 23:312-330.
- Souesme G, Martinent G, & Ferrand C (2016) Perceived autonomy support, psychological needs satisfaction, depressive symptoms and apathy in French hospitalized older people. Archives of Gerontology and Geriatrics 65:70-78.
- Williams GC, Rodin GC, Ryan RM, Grolnick WS, & Deci EL (1998) Autonomous regulation and long-term medication adherence in adult outpatients. Health Psychology 17(3):269-276.

Varsha Reddy Jayar
MGM Institute of Health Sciences, India
Title: Heat and spice in later years of life
Time : 17:35-17:45












